Prof. Dan Peer
1st time in the world TAU researchers destroyed most cancer cells in the bone marrow
Breakthrough in combating multiple myeloma:
For the 1st time in the world researchers destroyed most cancer cells in the bone marrow using a targeted system containing RNA therapy
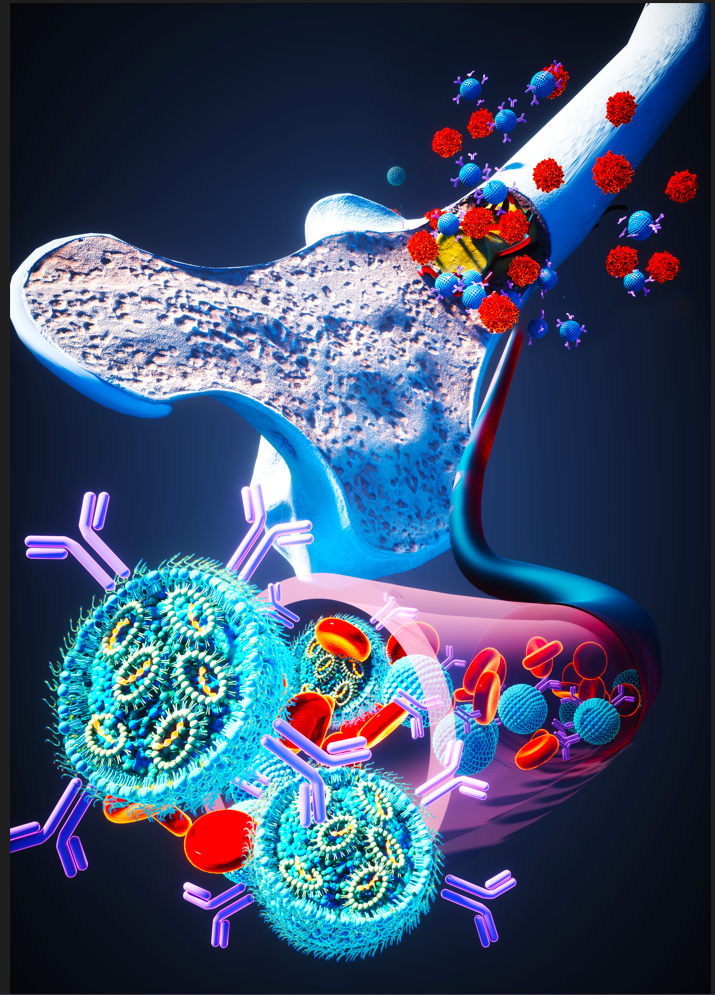
The researchers developed targeted lipid-based nanoparticles, similar to those used in the COVID-19 vaccine, containing RNA molecules that silence the gene CKAP5, encoding the cytoskeleton-associated protein 5. Once this protein was inhibited the cancer cells were unable to divide and died.
The researchers: “The targeted drug delivery system we developed is the first to effectively reach cancer cells inside the bone marrow.”
Researchers at Tel Aviv University destroyed 90% of the multiple myeloma blood cancer cells under laboratory conditions, and 60% in human tissues taken from patients at Rabin Medical Center (Belinson Hospital), using an RNA-based drug delivered to the cells by targeted lipid nanoparticles.
The researchers developed lipid-based nanoparticles (similar to those used in the COVID-19 vaccine) containing RNA molecules that silence the gene CKAP5, encoding cytoskeleton-associated protein 5. With this protein inhibited the cancer cell is unable to divide, which essentially kills it. To avoid damaging noncancerous cells, the nanoparticles were coated with antibodies that guided them specifically to the cancer cells inside the bone marrow.
The breakthrough was achieved by a group of researchers from Tel Aviv University and the Rabin Medical Center, led by Prof. Dan Peer, a pioneer in the development of RNA therapeutics and Head of the Nanomedicine Laboratory at the Shmunis School of Biomedicine and Cancer Research, also serving as TAU’s VP R&D, and by PhD student Dana Tarab-Ravski. The results were published in the leading journal Advanced Science.
Dana Tarab-Ravski explains: “Multiple myeloma is a blood cancer usually found in the older population. While most blood cancers appear in the blood stream or lymph nodes and spread from there to the rest of the body, multiple myeloma cells appear and form tumors inside the bone marrow – and are therefore very hard to reach.”
The study’s findings are very encouraging: under laboratory conditions, where cells are grown in flasks, the nanoparticles developed by the researchers eradicated about 90% of the cancer cells. At the second stage, the new treatment was tested on cancer samples taken from multiple myeloma patients at the haemato-oncological ward of the Rabin Medical Center. The success rate in these samples was 60%. Testing the ability of the nanoparticles to reach the bone marrow in an animal model, the researchers found that after a single injection the RNA had penetrated to 60% of the multiple myeloma cancer cells in the bone marrow. Lastly, examining the therapeutic effectiveness of the nanoparticles in the animal model resulted in eradication of two thirds of the cancer cells, and the animals showed significant improvement in all clinical indicators.
“People with multiple myeloma suffer from severe pain in their bones, as well as anemia, kidney failure, and a weakened immune system,” says Tarab-Ravski. “There are many possible treatments for this disease, but after a certain period of improvement most patients develop resistance to the therapy and the disease relapses even more aggressively. Therefore, there is a constant need for developing new treatments for multiple myeloma. RNA-based therapy has a great advantage in this case because it can be developed very quickly. By simply changing the RNA molecule a different gene can be silenced each time, thereby tailoring the treatment to the progression of the disease and to the individual patient. The challenge in these treatments is to reach the right cells. Today RNA therapeutics are approved for treating a genetic liver disease and for vaccines injected into the muscle, as we saw with the COVID-19 vaccines. The drug delivery system we developed is the first that specifically targets cancer cells inside the bone marrow, and the first to show that silencing the expression of CKAP5 gene can be used to kill blood cancer cells.”
Prof. Dan Peer: “Our technology opens a new world for selective delivery of RNA medications and vaccines for cancer tumors and diseases originating in the bone marrow.”
The clinical team included Dr. Tamar Berger, Dr. Iuliana Vaxman and Prof. Pia Raanani from the Institute of Hematology, Rabin Medical Center, Beilinson Hospital Petah Tikva 4941492, Israel
The research was funded by the the Boaz and Varda Dotan Hematologyoncology Center at Tel-Aviv University and by Lewis Trust for Blood Cancer Research awarded to D.P.
Link to the article:
https://onlinelibrary.wiley.com/doi/10.1002/advs.202370141
- Cover image for Advanced Science credit: Ella Maru Studio
- Prof. Dan Peer credit: Tel Aviv University
(Tel Aviv University grants permission for the use of these photos/images for stories about TAU research).